
What follows will be a specific description of various peripheral pulses and where to find them. It is often relevant to compare bilateral pulses for symmetry as well as the difference between upper and lower extremity pulses. The choice of where to palpate a peripheral pulse is dependent on factors including the patient’s age, body habitus, and the clinical situation (e.g., resuscitation, routine vitals at an office visit, evaluation for peripheral arterial disease, etc.). If relevant, the clinician can auscultate the heart while palpating a peripheral pulse to ascertain if every pulse gets transmitted as a palpable beat. Generally, 15 seconds is the minimum amount of acceptable time (multiplied by four to get the number of beats per minute) with more extended periods probably producing greater accuracy. Finally, the rate can be measured: the clinician observes a timepiece while counting the total number of palpable beats that occur during a predetermined amount of time. After noting intensity, the clinician will turn their attention towards the rhythm, feeling long enough to be certain that the only variation in rhythm may be the minor fluctuation that occurs with the respiratory cycle. Zero refers to a nonpalpable pulse, 1+ is a barely detectable pulse, 2+ is slightly diminished but greater than 1+, 3+ is a normal pulse and should be easily palpable, and 4+ is “bounding” (e.g., stronger than normal). By convention, “plus” always follows the number (e.g., 1+). The intensity of the pulse is noted and subjectively graded on a scale of 0 to 4. If possible, the limb under evaluation should have support throughout palpation.Įvaluation begins with an initial gestalt about whether the pulse is bounding or weak, fast or slow, irregular or regular, and equal or unequal bilaterally. (NB: although one often hears that utilization of the thumb for measuring pulses is less accurate secondary to increased perception of the clinician’s own pulsation during palpation, the author could not find data to support or refute this claim).
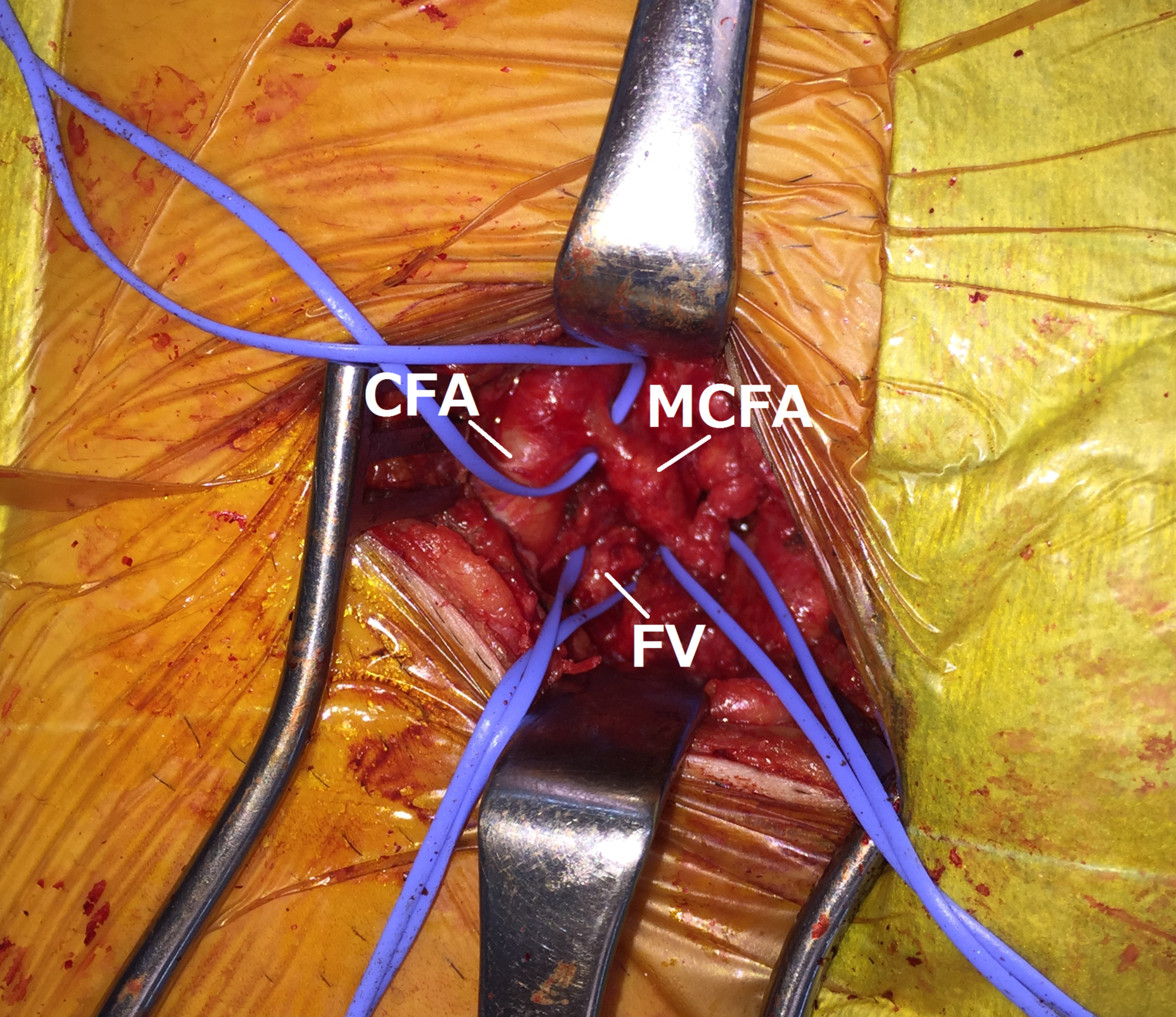
#FEMORAL PULSE SKIN#
Pulses are accurately measured when the clinician places their fingertips onto the skin overlying the vessel (locations, see below) and focuses on different aspects of the pulse. Pathological conditions can alter the rate, rhythm, intensity, and symmetry of the peripheral pulses, a fact that physicians can exploit when evaluating a patient. Besides the normal variation in a rhythm that occurs with the respiratory cycle, the heart rate should be regular in the absence of pathology. For example, colder temperatures cause vasoconstriction leading to decreased intensity.
The intensity of the pulse is determined by blood pressure as well as other physiological factors such as ambient temperature. This phenomenon guides many of the clinical uses of the attribute of “intensity” when evaluating pulses.Ī normal heart rate (HR) is determined by age (younger patients have higher HR), setting (exertion generally increased HR), and status of respiration (HR increases with inspiration). Higher pressures lead to greater palpated intensity as the peripheral vasculature distends more forecfully and to a higher degree. This waveform is propagated throughout the arterial system and can be felt and seen easily in several areas of the periphery. The subsequent release of that distention somewhat sustains the systolic wave of blood throughout the body, creating a spike followed by a downward sloping plateau in pulse waveform. This high-pressure wave distends the arteries, especially compliant “elastic” or “conducting” arteries, which tend to be larger and closer to the heart. Finally, modern medical technology allows for evaluation of pulses in ways beyond palpation, such as using Doppler ultrasound to characterize the pulse waveform further.ĭuring systolic contraction of the heart, a high amplitude wave of blood gets ejected through the aortic valve out towards the periphery. Peripheral pulses can be used to identify many different types of pathology and are therefore, a valuable clinical tool. Palpation occurs at various locations of the upper and lower extremities including the radial, brachial, femoral, popliteal, posterior tibial, and dorsalis pedis arteries and most commonly evaluates the rate, rhythm, intensity, and symmetry. This phenomenon is readily palpated and serves as a useful clinical tool, comprising one of the most commonly performed physical examination maneuvers at every level of medical care. A peripheral pulse refers to the palpation of the high-pressure wave of blood moving away from the heart through vessels in the extremities following systolic ejection.


 0 kommentar(er)
0 kommentar(er)
